1 Step Forward, 3 Steps Back
By Dusty Autumn York
Content warning: mentions of self-harm, suicide, suicidal ideation and substance abuse.
Photo by Tamara Shchypchynska via Unsplash.
When it comes to mental health, every step forward feels like taking three steps back. We have moments where we feel on top of the world, only for the world to come crashing down on us. Everyone experiences this, sure, but my steps always felt steeper. So much so that, as I climbed up one, I'd be knocked down with ease. Growing up, I was always called overly sensitive. I cried the moment it felt like the room grew tense. When I was angry, I couldn't control myself. My words spewed out like a poison I'd later regret putting in your drink. Losing friends who moved away or to conflict ripped me into a thousand tiny pieces I couldn’t put back together. I lived this way my whole life, never knowing any better or why I couldn’t take that first step forward.
It wasn't until February 2023 that I would be given insight into why I acted the way I did. I remember sitting in the psychiatrist's office, anxiously squirming in the old wooden chair as they read to me the results of my mental evaluation. My chest felt raw and hollow from the breakup that led me there. When I received that text, it felt as though my heart was being stabbed a thousand times. I felt like I was dying. I wanted to die.
What was the point anymore? If someone I loved didn’t want me, why should I want me? It was genuinely the worst pain of my life. The pain was real, real enough for me to grip onto a bottle of ibuprofen and take one after another as I prayed for the pain to stop. This, if you hadn’t guessed, was the incident that led my therapist to send me to the crisis center on campus. After what felt like a hundred questions, I was sitting in front of the man who would change everything for me.
"So, now that we have finished your assessment, we have a few diagnoses for you,” my new psychiatrist told me, thumbing through his written notes. He mentioned that I had severe major depressive disorder and generalized anxiety disorder, which wasn't a surprise. I had self-diagnosed myself with both since I was thirteen. What surprised me was that he kept going. "You also show clear signs of something known as borderline personality disorder."
My jaw dropped. A thousand thoughts were circling like vultures in my mind. A personality disorder? What did that even mean? What did it mean for me?
"Now, don't go home and Google borderline personality disorder. I've had too many clients immediately go to Google and freak out," warned my psychiatrist.
Of course, I didn't listen.
The first thing I did when I left his office was open up Google on my phone. This innate curiosity begged me to understand everything in my world. And it was a good way to take my mind off everything I was going through.
According to Google, this is the definition of borderline personality disorder:
So, what does this mean exactly? Well, the term “borderline personality” was coined by Adolph Stern in 1938. He used this term to describe a group of patients who didn’t quite fit into the psychotic or psychoneurotic groups. He used “borderline” to describe the patients because they “bordered” on conditions. The National Institute of Mental Health described it as “a mental illness that severely impacts a person’s ability to manage their emotions.” They also say that borderline personality disorder is often comorbid with depression, anxiety, eating disorders, PTSD, substance abuse and bipolar disorder. It’s honestly pretty rare to see someone with BPD not have one or two of those disorders along with it. There are a lot of symptoms attached, such as intense mood swings, the uncertainty of how they see themselves, black-and-white thinking, intense and unstable relationships (idolizing a loved one in a moment, devaluing them the next) and an intense fear of real or perceived abandonment.
It felt like I had found the missing puzzle piece that explained why I was who I was. Which is great, but the only problem was this feeling of guilt and anger blossoming inside me. I felt guilty for all the people I unknowingly hurt and for the relationships that I ruined with my overwhelming fear of the other person leaving. Maybe I had the answer but I didn’t know how to accept it.
Days turned into weeks after learning about borderline personality disorder, otherwise known as BPD, and I found comfort in talking about it with friends and family. I learned some of my closest friends also had it after telling them about my psychiatrist appointment. I also remember texting my brother, Kellin, and we bonded over our long list of mental health diagnoses when he told me he was diagnosed with it, too. This helped alleviate the stigma associated with BPD in my mind. In our society, borderline personality disorder is heavily stigmatized. People with BPD are unnecessarily characterized as “manipulative,” “attention-seeking” and “dangerous” by clinicians, which can make getting help challenging. People see us as “too unstable” and “too sensitive” to be around, which isn’t the case. In reality, we just struggle with controlling our emotions, something that can be made easier with a little compassion and therapy.
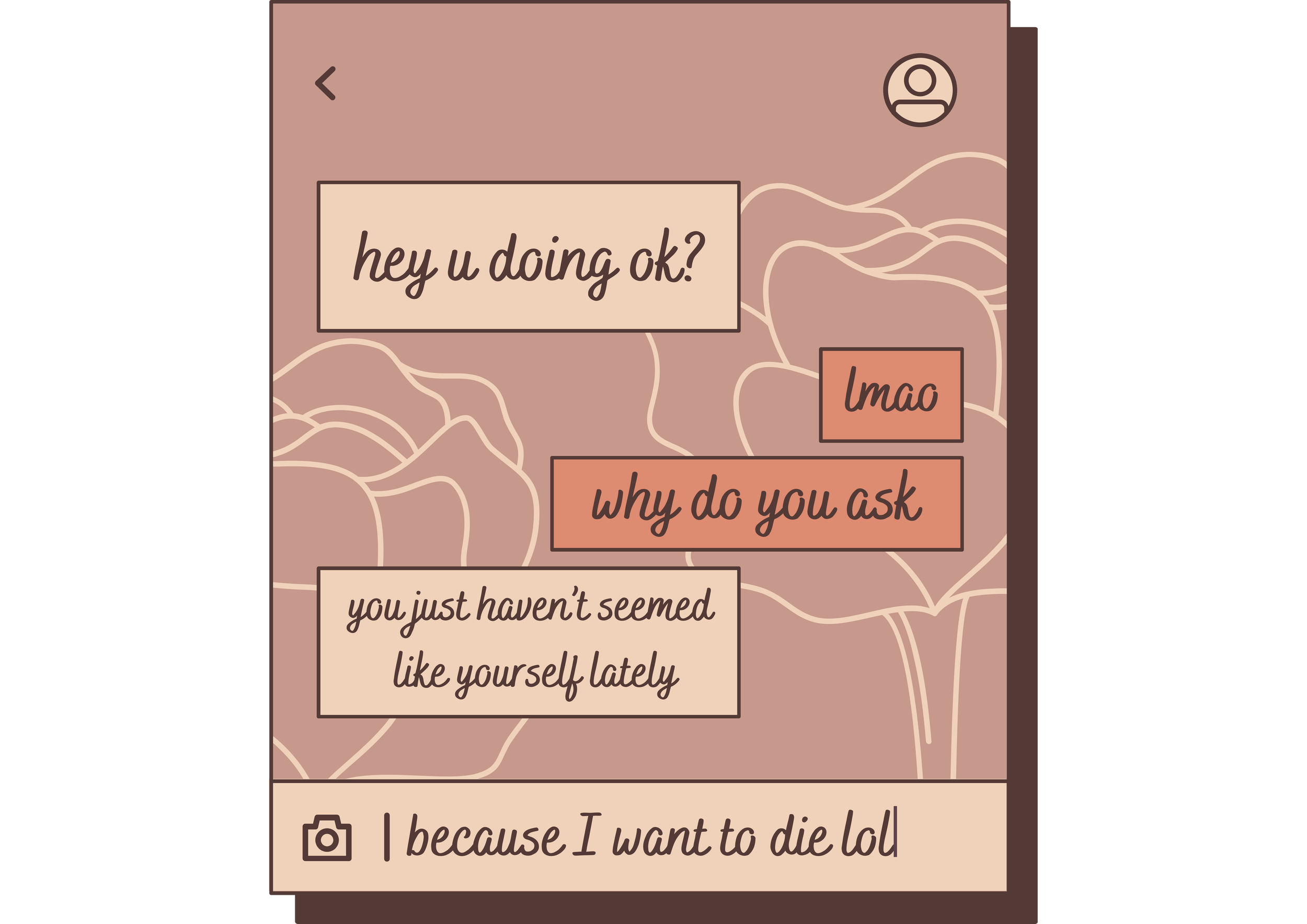
BPD manifests differently in everyone who has it. There are four widely accepted subtypes of the disorder: impulsive, discouraged or quiet, self-destructive and petulant. Each of these types emphasizes a different aspect of it. Someone with impulsive BPD, like my brother, experiences a high need to act impulsively without thinking, such as spending too much or overusing drugs and alcohol. Someone with the petulant type often experiences outbursts of anger and feelings of being unloved. For myself, I lean between discouraged and self-destructive BPD. Most professionals would call the discouraged type “high-functioning,” though I don’t think the term is accurate. We may not outwardly show our symptoms as much but they still affect us in other ways. Those of us with the discouraged type have an intense fear of abandonment, to the point where we would do anything to prevent it from happening, even going as far as threatening suicide to keep the person around. As much as I’m not proud of it, I have done this myself. Not in a purely manipulative way but as a last-ditch effort to keep them around to see if they care.
For many with BPD, these are not just threats. Completed suicide happens in 10% of those with the disorder, while 75% harm themselves in destructive ways in response to abandonment or rejection. For me, I don’t voice these thoughts out loud. Instead, my mind tells me that it’s better to be dead than to live without them, even though it isn’t better at all. We also internalize our anger to the point of blowing up on those we love. I’ve lashed out at friends, only to have overwhelming guilt for my anger.
As for the self-destructive type, it's exactly how it sounds. We often have thoughts of self-harm and self-destructive behaviors. We tend to have a strong hatred for ourselves and a warped sense of self. I habitually see myself as a monster, a horrible, disgusting beast that needs to be defeated. Some of the symptoms associated with this type include depression, suicidal thoughts, excessive self-criticism and abusing drugs and alcohol.
In the early days of my recovery, I used alcohol to help numb my intense mood swings. While it wasn’t healthy, it felt less destructive in my mind. It did help at times but I quickly spent days skipping class to wallow in my emotions while drinking one drink after the other. I’d find myself drinking from the early morning to late into the evening. I’d misuse sleeping medication because sleeping was my only escape. Even though I started medication for depression and anxiety and saw a therapist regularly, it still felt like I was being engulfed in the waves of my emotions strong enough to pull me under. Whatever step I had taken didn’t matter anymore. I was constantly starting over.
I remember reaching my breaking point at the beginning of March 2023. In the weeks before, I had many mental breakdowns and felt like I couldn’t control my emotions. My antidepressant at the time made me feel numb and everything all at once. I genuinely felt like I was going crazy and walking around like a zombie. All I knew was that I wasn’t myself.
The night before everything, I wrote a long text message to an ex saying how much I missed them. It was a moment of weakness, and I didn’t want to believe it was over yet, but it was. The next morning, I spent all day never hearing back. I felt myself breaking down to nothing. It was as if I was so numb that I couldn’t feel a thing. It was all so foggy. I remember dissociating in my room, only to come back into consciousness in the middle of an attempt. This was my breaking point, something I saw everything leading up to. But I wanted to live, which is why I walked from my room to the emergency room at Boone Hospital. I remember being asked what I needed to be seen for and saying that I was suicidal. I remember sitting in a room with a babysitter waiting for a psychiatric ward that was ready to take me. I remember the paramedic strapping me into the ambulance, telling me to hang in there when he passed me off to the local psychiatric center. I remember so much for such a traumatic situation.
The psychiatric nurses led me to wait on the children’s side while they set up a room for me. I made friends with one kid in his late teens who came to talk to me when I was alone. We bonded over paint thinner and chess for half an hour before he was discharged. Suddenly, I had nobody and the silence was deafening. Everyone was asleep when they finally took me back to the adult ward. The TV played in the background but it wasn’t enough to drown out my thoughts. I thought about everything that brought me here, the loneliness that demanded to be felt, and I was tired. I was tired of not being heard and feeling crazy about my emotions. I was fighting a war with myself without a single strategy and losing.
It all sounds dramatic. I know it does, but that's how I felt. I felt so strongly that my life was in danger and my sadness turned into physical pain. This is a shared experience that most with borderline personality disorder experience.
According to BPD specialist Marsha Linehan, “People with BPD are like people with third-degree burns over 90% of their bodies. Lacking emotional skin, they feel agony at the slightest touch or movement.” Every emotion is painful. Anger feels like rage. Sadness feels like depression. Being abandoned feels like mourning a loss. We live at these extremes every day because of the trauma we faced as children or the environment we grew up in. Not only that, but those with BPD are among the highest risk for suicide because of how painful it is. It's a never-ending fight for our lives.
I remember lying down that first night in the psychiatric ward in the harsh, cold bed. There were no curtains over the window and I looked up at the deep blue night sky until my vision blurred from my tears. I let everyone down. I tried hard to get better but it didn't matter. Nothing I did was good enough. It was in this sobering moment that I realized how alone I was. There were people in my corner who didn’t know I was in there. But a large part of me felt abandoned. Were they not wondering where I was? Did they even notice or care? I didn’t know but these thoughts plagued my mind until I fell asleep.
The next day, I spent most of it trying to entertain myself with puzzles until they authorized me to be discharged. The whole time, I just kept thinking about everything I was missing: classes, lunch and gaming with my usual coffee from Stars. Most of all, I missed all my friends. So much so that I lied to get myself out sooner. They switched my meds in the morning and, after a long afternoon of puzzles I couldn’t solve, they escorted me out into the waiting room where two of my closest friends stood waiting for me. Without a second thought, I ran up to them and hugged them. I didn’t want to let go because letting go would mean I’d be alone. “You guys are here,” I said happily.
“Of course we are. We’re always here for you,” one friend said. “Now, are you ready to go home?” And just like that, we walked out of the hospital, side by side, feeling less alone than when I arrived.
Since being released from the psychiatric ward, I've taken many first steps. I started seeing a therapist who helped me explore my intense feelings and she even taught me how to cope in healthier ways. I advocated for myself with my psychiatrist to get prescribed medication that would help me and it did. The combination I’m currently on has lessened the painful symptoms I experienced drastically. I also became more aware of how BPD affects me and I've learned how to communicate with the ones I love about what I am going through. Of course, I’ve had many setbacks, but I didn't allow myself to go through them alone. People come and go, even the good ones, but, from the words of Taylor Swift, “everything you lose is a step you take.” Recovery can be challenging, regardless of your diagnosis, but it's possible. You just have to take the first step.
If you or a loved one is struggling with depression, suicidal thoughts or substance abuse, call or text 988, or contact the SAMHSA hotline at 1-800-662-4357.